YOUR MEDICAL MICRO-ROBOT IS READY — WITH BRAD NELSON
ROBOT THROMBECTOMIES AND DRUG DELIVERIES INSIDE THE BRAIN
October 26 2025—Microscale robots will be conducting medical procedures inside our bodies sooner than you think. That’s the big takeaway from my fascinating conversation with Prof. Bradley Nelson, head of the Multi-Scale Robotics Lab at ETH Zürich. For those of us who grew up watching Fantastic Voyage, that's a stunning statement!
Brad has spent more than 40 years researching and building robots. He has won numerous awards in robotics, nanotechnology, and biomedicine and was named to the "Scientific American 50" list for outstanding acts of leadership in science and technology. His lab is undefeated international champion in Robocup's Nanogram Soccer League and he is in the Guinness Book of World Records for the "Most Advanced Mini Robot for Medical Use."
Brad discusses the lab’s bio-inspired prototypes and associated innovations in propulsion, power-delivery, external control and biocompatibility, the special challenges of fabricating and operating robots at these scales, and how all these developments are now converging into tiny robots capable of performing thrombectomies and precision drug deliveries to brain tumors.
We then explore regulatory considerations and the future ‘democratization of surgery’ benefits that Brad aims to unlock adding telesurgery capabilities and more autonomy.
Click the audio below to listen. It’s an inspiring journey into the (near) future of robot medicine!
And as always, scroll down for my post-conversation reflections and a full transcript, and don’t forget you can listen to more pathways to a better future from the world’s leading scientists and innovators by subscribing to “FutureBites With Dr Bruce McCabe” on Spotify, Apple, or on your favorite podcast platform.
My special thanks to Brad for generously hosting me and sharing his insights, and also to Oliver Brinkman for kindly taking time away from his research to show me around the lab.
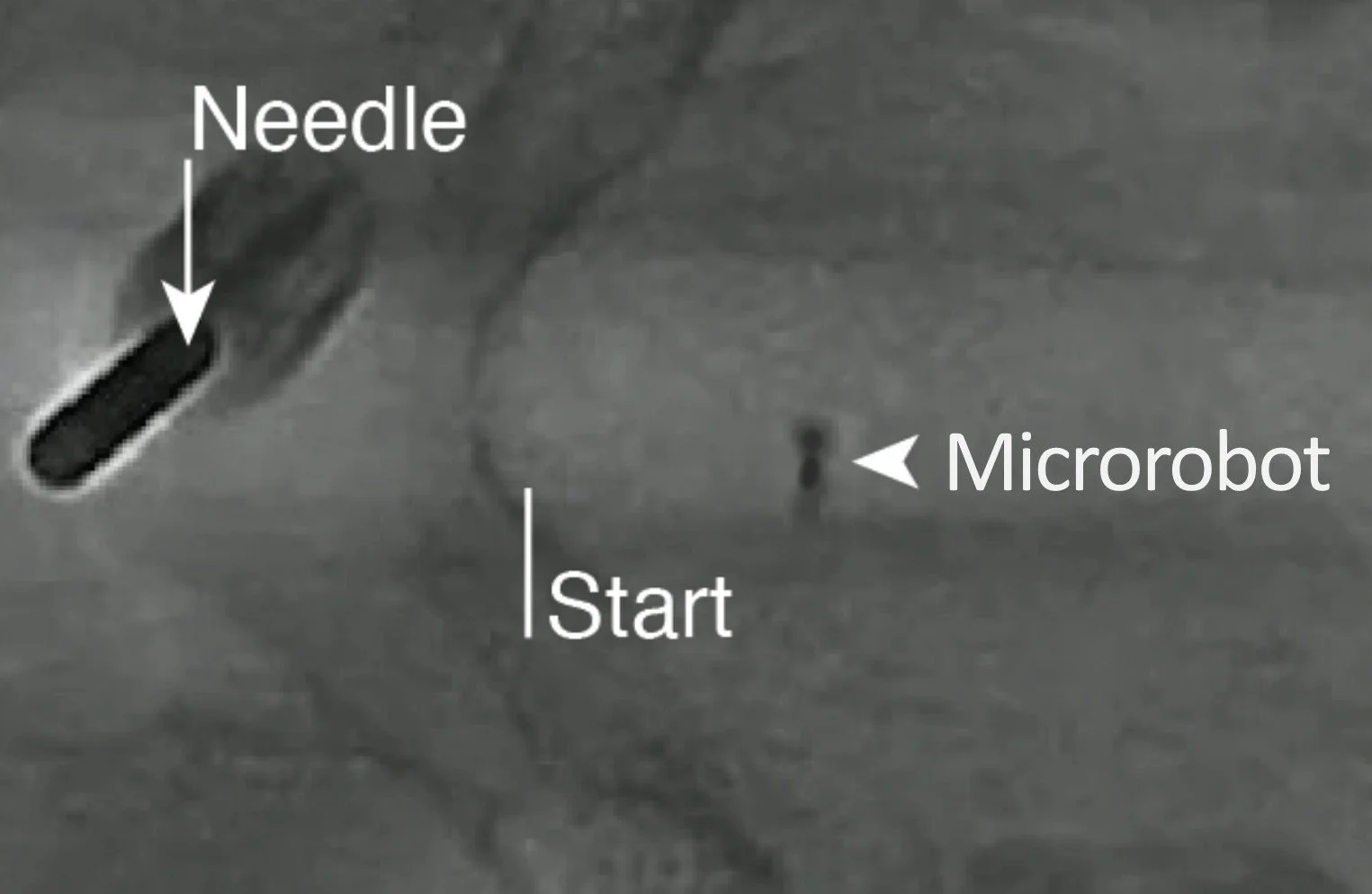
Cover image: In vivo evaluation of the robotic platform in a clinical setting. From “Clinically Ready Magnetic Microrobots for Targeted Therapies,” Landers et al, https://arxiv.org/pdf/2501.11553
PATHWAYS TO A BETTER FUTURE
MEDICAL MICRO-ROBOTS IN HUMANS SOON
The biggest message from our conversation was that we will have micro-scale robots operating inside humans soon. All of the component parts are built. Successful tests have been conducted inside the blood vessels of pigs. The main task now is securing regulatory approvals for the first systems and procedures.
Of course we are not talking miniaturised submarines with miniaturised crewmembers like those that featured in Fantastic Voyage; the genius in what Brad and his colleagues have developed — and it is genius — is supplying the required power and navigation from outside the body, using magnetic fields.
But human-supervised, microscale robots will be swimming through our arteries and into our brains to perform thrombectomies and micro-targeted drug-deliveries.
In vivo evaluation of the robotic platform in a clinical setting. From: “Clinically Ready Magnetic Microrobots for Targeted Therapies,” Landers et al, https://arxiv.org/pdf/2501.11553
FIRST TARGETS: THROMBECTOMIES AND PRECISION DRUG DELIVERIES
Brad and his colleagues have made thrombectomies for stroke patients their first target. Manual surgical procedures for thrombectomies already exist, but they demand extremely high surgical skill levels held by a limited number of surgeons and available at a limited number of clinics. By contrast, the number of stroke-sufferers globally is huge and according to Brad only a tiny fraction (less than 3%) receive that kind of intervention.
Micro-robots offer an alternative surgical system that can more easily and precisely deliver an enzyme or interact mechanically to break up the blood clot. This offers a game changer by “allowing qualified people to do more complicated procedures with less training, and therefore [greatly] expanding the number of patients that get treated.” The footprint can be widened still further with the addition of satellite links and telesurgery capabilities.
This same “democratizing of surgery” goal, incidentally, featured in my recent conversation with Philipp Fürnstahl about multi-sensory robots for orthopaedic surgeries. In both cases, the biggest health system benefits of roboticization are not so much about making existing surgeries safer and more about scaling the number of safe surgeries.
The other near-term target is precision-delivery of drugs to glioblastomas and to diffuse intrinsic pontine gliomas.
In all of these cases the lack of treatment options for patients also translates to a greater willingness of regulators to consider experimental procedures, an important factor when selecting first targets.
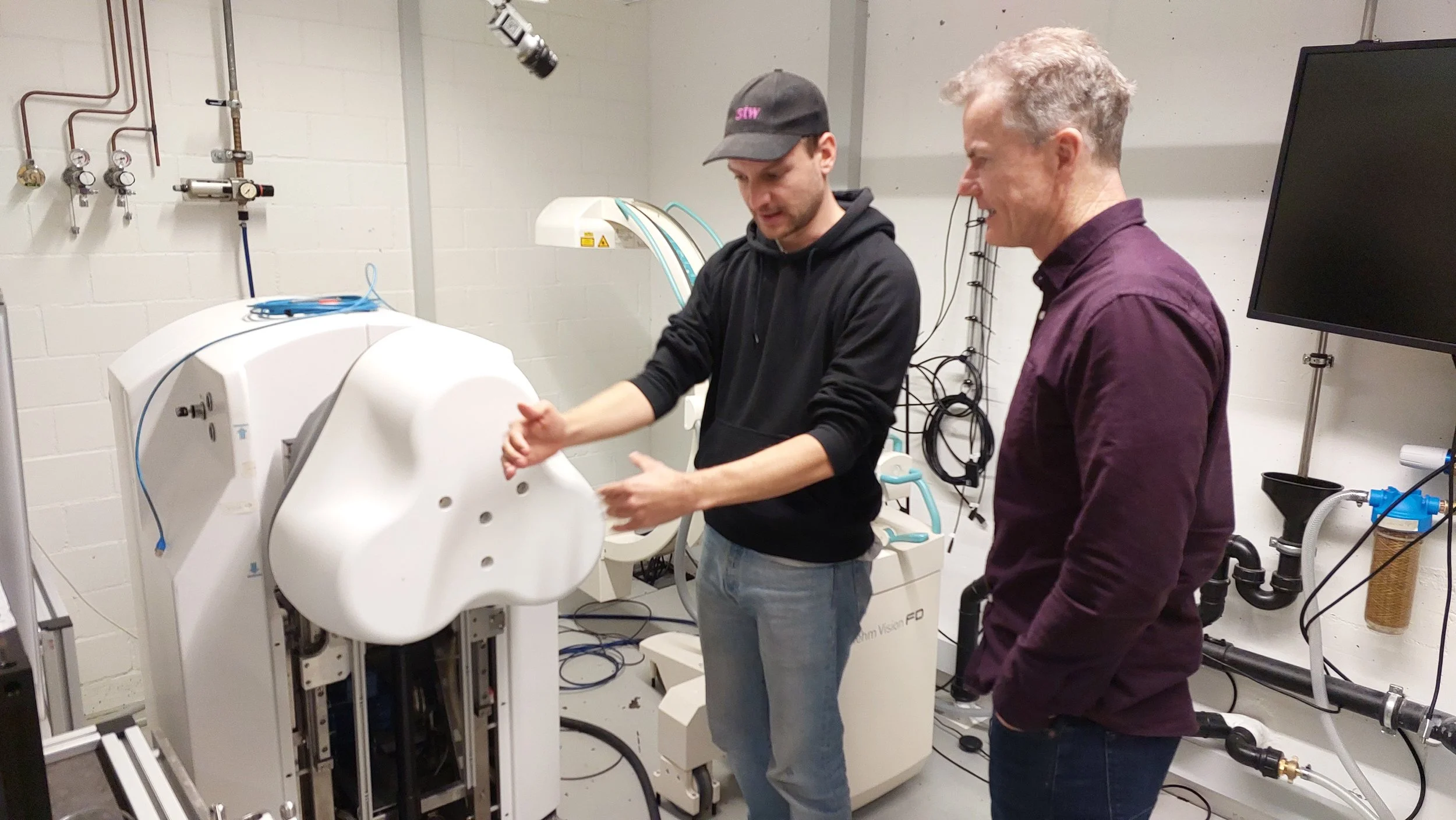
Oliver Brinkman explaining the magnetic system developed at the Multi-Scale Robotics Lab for powering and navigating micro-robots through the patient’s vascular system to the target.
BIO-INSPIRED & MULTI-DISCIPLINARY
The Multi-Scale Robotics Lab is a showcase for bio-inspired innovation. Again and again solutions to problems have come from examining the ‘solutions’ evolved in life, such as flagella-propelled bacteria and the shape changing trypanosoma brucei parasite. Clearly, there are endless more possibilities to be mined. As Brad put it, “it's fascinating to understand first of all how nature solved the problem [but in addition] our advantage as engineers is we're not as constrained as nature in our solutions.”
The lab is also a first-class demonstration of what true multi-disciplinary teams can accomplish. Chemists, mechanical engineers, fluid dynamists, magnetic field physicists, materials scientists, polymer and nanoparticle specialists, 3-D printing specialists, medical specialists, and of course computer scientists have all collaborated to build these systems. This was especially salient in our discussion of robots designed for post-op retrieval versus robots designed for biodegradability. The sequence of considerations to make fully-functional robots that were also biodegradable went something like this:
Three magnetic elements to choose from … Avoid toxicity … Which alloys can be made with iron? … Which of those alloys have the desired properties? … Which polymers are bio-absorbable? … Which materials will show up on the fluoroscope? … It is possible to manufacture this? … Can we manufacture these at scale?
As I say, first-class. It must be an exciting place to work, and I’ll bet most lab-leaders would kill to be able to apply all those capabilities to one problem!
THE FUTURE: MORE SENSING AND MORE AUTONOMY
Brad did not shy away from my questions on long-term future possibilities, and while adding more sensing and more autonomy to microrobots might seem ridiculously hard (how to add accessories at micro- and nano-scales?) consider:
The MSRL has already advanced from (a) dumb instruments manually inserted and manipulated at the end of long guide-wires, to (b) robots that can twist and turn their way forwards through blood vessels dragging the guide-wires behind, to (c) untethered microrobots that swim to targets using externally supplied power and navigation.
We know that more kinds of sensing, autonomy, and action are possible at micro- and nano-scales, because bacteria do it all the time.
I particularly like Brad’s idea of homing in tumors based on different pH levels and temperatures. Also interesting was Brad’s comment that “anything applying force,” such as stitching, was an especially tough problem for tiny robots.
Bottom line: many more surgical possibilities yet to be explored. Perhaps one day we’ll have those new robot-enabled procedures we discussed to remove retinal vein occlusions, deliver age-related macular degeneration (AMD) drugs ultra-precisely to the retina, and to fill aneurysms.
Holding a vascular system mock-up for testing micro-robots at the Multi-Scale Robotics Lab
MORE TO EXPLORE
The following links kindly shared by Oliver Brinkman:
Microcapsule for stroke treatment (preprint, peer-reviewed; publication to follow soon)
Nanoflex robotics - commercializing electro magnetic navigation systems for endovascular procedure
And be sure to check out the Multi-Scale Robotics Lab website and Youtube channel.
INTERVIEW TRANSCRIPT
Please note, my transcripts are AI-generated and lightly edited for clarity and will contain minor errors. The true record of the interview is always the audio version.
Bruce McCabe: Welcome to FutureBites, where we look at pathways to a better future. I'm your host, Bruce McCabe. Today we're exploring robots, but not just any robots, very small robots. We're here at the Multi-Scale Robotics Lab and my guest today is the head of that lab, Professor Bradley Nelson. Welcome to the podcast.
Bradley Nelson: Thank you. It's a pleasure to be here.
BM: Thanks for making time. Very excited to talk to you about your work because I've been seeing it from a distance for a long time. You are working at very, very small scales. But before we get to that, just to introduce you, you're the head of this lab at the Federal Institute of Technology here in Zurich ETH. You've been doing robotics for more than 30 years, looking at your profile.
BN: More than 40 years now.
BM: More than 40. Need to update that profile!
BN: I started reading robotics research papers in 1984, so that was my master's degree. Yeah. Yep.
BM: Fantastic. I wasn't even in undergrad by that stage. It was shortly after that. But there were some fun things when I was reading your bio, just looking at that career, apart from being named in Scientific Americans 50 list for outstanding acts of leadership and science, things like that, your lab was, as at the last update, undefeated in the RoboCups Soccer League. Is that still the case? They still hold that?
BN: Yeah, yeah. They did a two or three, I think they did two competitions. It's hard to compete. It's hard to make these things work. And we were playing on about the size of a grain of rice, was the pitch.
BM: It's the nano scale soccer.
BN: It was small and it was a great challenge for the group and for the lab.
BM: And the other lovely thing was, you list there as being in the Guinness Book of World Records for the most advanced mini robot for medical use. I wonder whether you've even got more advanced and more mini since that was awarded.
BN: Oh, yeah. Yeah. That was quite a while ago. So we just keep going down the path trying to make these things more intelligent. We think of what they're going to do and we're going to be having an important paper coming out soon on how we're actually now able to control these at clinical scales, that is at human scale, so we can actually move these things around inside. A lot of the work you've seen over the last 20 years or so often are under microscopes and everything's right around there. But now we're able to do this at large scales and that's a big challenge.
BM: I want to get into those propulsion systems and how you control them and that sort of thing. Just before we get to the technology though, yourself, 40 years, was there a particular thing or event or person who inspired you to go down this path? Or was it your sci-fi reading as a young man?
BN: Well, let's see. I was seven years old when they landed on the moon, 1969. And I think there's a lot of people from my age range that developed an interest in engineering space. If you look at the Elon Musk's and Jeff Bezos and Richard Branson's, everybody in this timeframe wants to get into space. And I think the space program probably, and watching that as a kid, encouraged a lot of us to get into science, math, engineering and that kind of stuff. And I ended up in mechanical engineering and then eventually kind of accidentally fell into robotics back in '80. Actually it was 1984.
BM: Yeah. Wow. Pretty early. I mean, robotics was the specialty pretty early.
BN: Yeah. And like I said, I was not intending to get into it. I wanted to get into control theory and something with a little more theoretical depth. But I found the problems in robotics were really hard and not well defined, which made them interesting, I think.
BM: Yeah. And one of the interesting things from an outsider's perspective is just how the problems are still hard, because we're pushing the boundaries so much now in sensory capabilities and other things. So, there's a lot more work to be done. I mean, there's another few decades worth of wonderful work still to come, right?
BN: Right. Right. And I think a lot of the public confuses robotics and AI, right.
BM: Especially now.
BN: They see the advances in ChatGPT and they falsely think, oh, this is going to translate right into robotics. And while robotics certainly benefits from a lot of that, I think the problems in robotics are fundamentally, they're mechanical, their interactions with the world. And so the complexity of that is much deeper than we understand. Just picking up this glass and moving it in my hand, that's really hard to model. And these simple things we do every day, we don't realize... I think Hans Moravec, who was a Carnegie Mellon when I was there, he has been given credit for something called the Moravec's paradox, which is that we can build robots or we can build AI systems that can beat world class chess champions, Go nd these games... But we still can't build robots that have the skills that a two or three year old has in interacting with the world.
BM: Yeah. We still can't build that general purpose assistant for the home to do all the tasks. Although one the Japanese fantasize all about is to build one that will help you as an elderly person, pop you into bed and all those good things. Very hard problems in three dimensions. So here we are talking about smaller robots. And I understand, although this lab is called the Multi-Scale Robotics Lab, mostly I associate it with very, very small robots, microscale and nanoscale. And is that accurate still? Or...
BN: Yeah. I think that's what we focused on. I came here to ETH in 2002, so I've been here 23 years, and that's where a lot of our work is focused is on how to make small, intelligent machines and figure out what they're going to do.
BM: And mostly for medical purposes? Is that where the main set of use cases is at the moment?
BN: Yeah. I think that's what we see as the biggest area that this could probably contribute to right away. We have worked in environmental cleanup and using these things to move through water and help dispose of toxins, but I think that's … the big use case people see is really going to be in healthcare.
BM: Yep. Yeah. Well, that excites me particularly. There's so many things going on in healthcare at the moment, people trying to rethink what they can do and what the opportunities are. So perhaps we could just get into some of the projects we've got underway, those micro and nanoscale robots. I wonder if you could maybe run me through some of the ones that are particularly inspiring or particularly thought-provoking in terms of possibilities that you're working on here.
BN: Yeah. So we first started thinking about this actually in 2003 when I got here. We started thinking, what's a grand challenge? And so let's try to make a small intelligent machine. And it started to get interesting when we started looking at microorganisms, things like flagellated bacteria, things like E. Coli that's got these little rotary motors that spin. And you look at that and we were thinking, why does it swim that way? What's the benefit of this rotary motor? But you look at the physics and the fluid dynamics and you realize, oh, wow, that is a pretty elegant solution to trying to make a small device move.
BM: Yeah. Because it's different at a small scale, right, movement and friction …
BN: Right. Exactly. The physics that predominates the way you interact with fluids, it's a laminar flow instead of a turbulent flow. You look at it and you're like, oh, nature's pretty smart to figure this one out. So we started making these things artificial bacteria flagella, and that's the thing that Guinness Book picked up that you mentioned before. And there's a lot of reasons we like these helical structures. There's a lot of benefits to the way they can move. And then we started thinking about shape-changing robots, things made out of polymers that could react. And we were inspired there by a parasite called Trypanosoma brucei, which is responsible for trypanosomiasis or the African sleeping sickness. But what intrigued us about this parasite was that it changed its shape at different points in its life cycle. It starts in the gut of a tsetse fly, bites a person, swims through the bloodstream, crosses the blood-brain barrier into the brain, and then starts reproducing and eventually kills the host. But we thought, how does that change its shape? And wouldn't that be useful for a robot to say carrying drugs? You want it to move, you want it to get to where it goes, and then you want it to stop. And so if we could make a robot that changed its shape that way.
So we got inspired by that. We got inspired... Started looking at, how might we program some of these in situ and change their magnetic properties? And so then we worked with Laura Heydermann. She's a professor at ETH and works at the Paul Scherrer Institute, one of the government labs. And her expertise is in nanomagnets, and we learned how we can reprogram nanomagnets differently. And so then we could actually re-encode the behavior in situ. So as this device is inside, we could change its behavior that way.
BM: Can I stop you there?
BN: Sure. Sure.
BM: Let's drill into that. Because I always thought you were controlling the propulsion externally to the body of these tiny robots. I guess they're experimental, they're not inside bodies at the moment. But the nanomagnets you're talking about are actually part of the device.
BN: They're on the device, yeah. So, there are different ways we can make small things move. Some people look at chemical propulsion. There's a lot of issues with the fuels they use, it can be toxic. Some people use light, but it's hard to get light into the body. And acoustics is interesting, ultrasound. So we've had some folks that have gone on, like Daniel Achmed now, who's in Bern now working on using ultrasound to move these. But I've always stuck with magnetics. I think magnetic fields make a lot of sense because we can project them in the body, we know they're safe. And so then we always, on our device, include some kind of a magnetic material, usually a type of iron that's biocompatible. And so that's the way we propel these.
BM: Okay. And you said reprogramming them as part of, do you mean externally reprogramming the way you hit them with magnetic waves or reprogramming something on the device?
BN: So in these, the one that I was talking about with Laura, we were actually reprogramming them in situ. So we would just blast them with different kinds of magnetic fields and they would remagnetize themselves as we wanted, and then they would start behaving differently. So we just, as a demo, we made a little origami crane about half the width of a hair. And then we could, the same crane, by reprogramming it, we can show it hovering or flying or moving in different kinds of ways. And so we keep looking at how we can make these more intelligent, respond to their environment ways. But it's not with a big robot where you just download some new kind of code, right?
BM: Yes. Yeah. You're working with a lot of constraints.
BN: So a lot of our expertise goes into the materials and the morphology, the shapes of these and what they can do. And then also in how we generate the magnetic fields to make them move through the body.
BM: Wow. I mean, it brings up questions instantly about materials and also being metabolized or something at the end of life. I mean, that must be a major consideration. Are all these designed on the basis of we want to retrieve them afterwards, or are they designed to dissolve when they're finished?
BN: Yeah. No. That's a big concern. So either you're going to have to get them out of the body, or for the small ones, we make them out of materials that are biodegradable. So they will be absorbed by the body after they're finished. And so that makes the problem a lot more challenging because you've got now a lot fewer types of materials you can use. There's three elements that are magnetic, nickel, cobalt, and iron. And well, you don't want to put nickel in your body, you certainly don't want cobalt hanging around in your body. Iron, we can tolerate. And then we make alloys of that. We use different alloys to get different kinds of properties. And so that limits our magnetic material. Then you have to look at your polymers, which of those are bioabsorbable or biodegradable. And when we put them in the body too, we have to think, well, how do you know where they're getting there, that they're getting where you want? So we have to put, usually we use x-rays to look into your body. And then we have to put a contrast agent on our devices so they can show up and get a good strong signal on the fluoroscope that's going to be observing them move through the body.
BM: That's still the case that x-rays will be your primary way of ...
BN: Well, a lot of what we're doing is in the brain. A lot of what we're doing is looking at treating blood clots and things like that. And that's the standard of care now is to use fluoroscopes to observe where the blood clot is and to look into the body that way. So that's a good way to do it for now.
BM: That's amazing. I want to come to that because I saw something online you won an award very recently for actually having a robot to do thrombectomies for stroke patients. That's just mind-blowing in itself. But let's just continue that story. So you started with propulsion and how to energize them and how to reprogram them. And have we finished that story? Are there other threads to that now?
BN: Well, there's two things to think about. One is the research and what's possible. And it's always fun to make these devices and just show surprising behaviors. But then the other side, after you've done this a while, is you want to actually make these useful. You want what we call translate. We want to translate it from the lab into the clinic, into the hospitals. And when you do that, you have to go back and make it simple. With like the KISS principle. Keep it simple and stupid. And so then all these lessons we've learned in our research, we pull those out and then we keep our devices as simple as we can and just do the minimum. Our MVP, our minimum viable product.
BM: Yes. Minimum viable product [laughter] It applies to robots too!
BN: And that helps obviously get over regulatory concerns. It helps if you're really trying to translate this. Well, you're going to need investors because of all of the expense of that. So you've got to make sure there's a return on investment. So, the problem gets more complicated than just trying to build a small robot. It's also trying to understand how... We work closely with doctors and surgeons.
BM: How it will be used, how people train on it.
BN: And you also have to think about the regulatory agencies like the FDA or NMPA in China or the CE Mark here in Europe. And what are their constraints and how do they see these and make sure that you've taken that into account in your device. And then, of course, like I said, it takes a lot of investment. So you've got to think about what diseases make sense, where there can be a return on that, where are the needs. And so it's a big puzzle to put together.
BM: I bet it is, but a wonderful challenge too. Can we start to put together a little mental timeline of what's at the early end of the horizon in terms of simpler procedures that might be approved first and what would be more aspirational as we push out?
BN: Yeah. I think right now people are looking at clinical applications. There's two things you see people looking at. One is treating stroke, ischemic stroke, these blood clots in the brain. 87% of strokes are from these blood clots that get lodged in your brain. It is the second leading cause of death in the world. One in four people are going to suffer a stroke at some point in their life. And if you suffer a stroke, you have a 77% chance of either dying or being permanently disabled. Big need there.
BM: Big target.
BN: And can you use this technology to help address that problem? It's a worldwide problem. There's a good therapy for this, a good procedure called a mechanical thrombectomy where they go in and actually remove the blood clot, but less than 3% of the people in the world are getting that therapy because...
BM: Why?
BN: You have to be at a stroke center. You have to be near a place that can support a stroke center 24 hours a day, seven days a week. That's very expensive. You have to get there as quick as possible because the more time this clot's there, the more brain tissue is dying. The surgeons say time is brain in these cases. You have to have experts, and there's just not enough expert surgeons in the world that can do these procedures. Now here in Zurich, I mean, I can look across the hospitals just a couple minutes away from me. There's a helicopter pad on top of it specifically to try to get people that are suffering from stroke and other diseases where time is important there to be treated. It takes a lot of infrastructure. And of the 8 billion people in the world, I think something like 5 billion don't have access to basic surgery and anesthesia, and a third of disease is amenable to surgery. So there's just a need to help distribute this widespread.
BM: So the standard way of doing it is to what? How do you get... Just quickly, I guess the brief form of how do you do that mechanically without a robot today with a specialized surgeon? You must drill through the skull or do you come up through a blood vessel and then cross in?
BN: Yeah. The standard of care is a mechanical thrombectomy. So the first thing is to realize you have a stroke. And so the acronym they use is FAST, and F stands for face, if your face is numb. A is for arm, if your arm is hurting. Speech is if you're slurry. Then T is time. If you realize you're having a stroke, you need to get to a hospital right away and they will diagnose it. They usually do a CT or an MR, a CAT scan or a magnetic resonance image to see it. Then they got to figure out where we're going to send you. If you're lucky, you're at a stroke center and they'll send you there. If not, they'll put you in an ambulance or helicopter and try to get you to one.
BM: And time is moving.
BN: And time is moving every something like every 30... What? Every hour delay is a 30%... There's data on how you're suffering this whole time. And so then what they'll do is they'll figure out where the... You'll get to the stroke center and they'll figure out where the blood clot is. They'll look at the data, the medical images, and they'll put a guide wire, a little guide wire that's around anywhere from 800 to 400 microns in diameter. So less than a millimeter inside. They'll put it into your femoral artery in your groin and they will snake it up about a meter or so deep into your brain to where the blood clot is.
BM: Got it.
BN: Then they put over that, they put a catheter that's got a... And that goes over the guide wire. They pull the guide wire out and then that catheter can suck out the blood clot. And it's great. It's a great way to treat it, but it has to be done quickly.
BM: And with all those disadvantages you explained.
BN: And it requires experts because you're dealing with blood vessels in your brain and you want to be very, very careful when you're there.
BM: So let's now look at the alternative. If we do it with a micro or nanoscale robot, how would that procedure work?
BN: Well, it would be similar, but instead of having to put the wire all the way up, you would be observing it and kind of driving it through your blood vessels like a self-driving car. And reach it and then you could have on that robot, you might have an enzyme that can help break up that blood clot. It can also have a mechanical interaction to try to destroy it. And so that's one of the things that a lot of folks in the research community are thinking about is stroke because it is so prevalent and there's such a need and people aren't getting the treatments they want. The other thing that folks are looking at, and there's some companies have gotten some funding to do this too, is to treat brain cancers. So things like glioblastomas and brain stem like diffuse pontine glioma. And some of these very aggressive brain cancers, there just aren't any good treatments for and the drugs that are used to treat them are very toxic.
BM: Yeah. And we don't want to soak the whole brain in those toxic.
BN: You don't want to soak your whole body in these things. And so that's the promise of micro robots is they can carry highly toxic but very localized amount of drugs. They put it just where you want it. And these are diseases where there's just really not treatment options. And so that also makes the regulatory agencies more forgiving in this when they realize that we don't have a lot of choices and they're more willing to go with a more experimental procedure in that. And so that also helps translate these in that sense.
BM: So in our theoretical timeline here, that would be a bit further out.
BN: Well, it could be, but it actually could be closer because the regulatory hurdles are less. The problem with stroke, the issue with stroke, is that we know what the best treatment is. And you don't want to offer somebody a lower quality treatment. So the regulatory agencies, you've got to show equivalency, and so that can make it harder to get out there. And I think with some of these other, what we call orphan diseases, that maybe don't have as big of a need, there's not as many patients with them, but there's definitely a need, then maybe you can get those across the regulatory barrier a little easier. And so that's why some folks are looking at that as well.
BM: Where are we at with the process? So mechanically, you feel capable of delivering, like just in the lab, capable of delivering those capabilities as a procedure. So is it now a multi-year process with the regulators to try and get this across the line? Is that where we're at, or are they missing mechanical and computer science elements still, or is that sort of you're starting to feel confident about that side?
BN: So the regulatory, a lot of this is a challenge because it's very new, and regulators and people don't know how to treat it.
BM: Of course.
BN: And so right now, it looks like the regulators look at this as a whole system rather than component by component. So instead of getting your robot approved, and then your electromagnetic navigation system that's going to put in the magnetic fields, and then maybe some of the other tools and the user interface, instead of doing those all individually, it's a system. And so then that also makes it a challenge.
BM: I bet. And I'll bet it's, what is... A lot of these things, even when I look at pharmaceutical products, it's a 10-year process from day one.
BN: Yeah. I mean, yeah, certainly several years, but 10, I think we're... You take these things in steps. And so the first therapies that we see, for instance, with stroke, will probably be robotically controlled mechanical thrombectomies in the classic way, but with robotic devices. So you're doing what the surgeons are doing right now, but you're doing them automatically. And then the next step will be, okay, maybe we can get rid of the wire and just put the device in itself. But those take time.
BM: Of course. But anyway, they're like the early targets. That's a kind of, if people are listening to this in healthcare and just wondering what the possibilities might be in this coming decade, they're the early targets.
BN: Yeah. Yeah. And when we work with our surgeons too and they start seeing what we do, then all of a sudden they start getting a lot of ideas. And so there are a number of issues people have in their brain with the way the blood vessels are, things like AVMs, arterial venous malformations. And there are ways you can go in and surgically deal with these. And they see possibilities for moving our devices in and helping treat things like AVMs or some of these other kinds of things that the public doesn't really know much about until you get one and then they realize...
BM: Yeah. That it's very urgent. Well, we touched on capabilities because one of the things I wanted to ask you about was the actions that can take place. So, one was a drug payload. One was bringing a catheter and sort of sucking the clot out. And these are possible at that micro scale. What else could we do? I mean, is cauterization an option? I'm thinking of a use case which may not be practical, but surgery and cauterization in the eye, for example. I don't even know whether it's a particularly suitable target for robots, but I once saw a demo of a small micro robot being placed into an eye, a bull's eye, I think it was. And I've got family members who have branch, what do we call it? Branch retinal vein occlusions and things...
BN: Right. Right. Right.
BM: Yeah. And you think, gosh, this is microsurgery in a very delicate environment. And I wonder if these are also targets or not.
BN: Yeah. So we've looked at things like you say, retinal vein occlusions you're talking about where, I mean, basically there are blood clots in the veins of your retina and that you just lose your sight. All the retinal cells just die and you can't see and you need to get in there rapidly. And so people have thought about that. How can we get these into these retinal veins? We've also looked at treating them. Leading cause of blindness in the Western world is age-related macular degeneration. And there are drugs that can slow or halt the progression of that disease, but they have to be administered every few months through an injection in the eye. And so we've thought of ways we might use these devices to deliver the drug directly to the retina right where the disease is, where the degeneration is happening and perhaps making it more effective and prolonging the need for the patient to have to keep going back to the hospital for.
BM: Is that a robot device or is that something you insert in a needle and you do your precision directly?
BN: Right now it's all done for AMD, for age-related macular degeneration.
BM: It's an injection.
BN: It's an injection. Right. And there is...
BM: I have to say, by the way, my father has this and he has the injections.
BN: My mother has it, has the injections, and my grandmother had it, and my sister had it.
BM: Quite common.
BN: So it's common. Like I said, it's...
BM: Terrible.
BN: Yeah. I think Roche has recently come out with what they call a port delivery system, where they actually put a little device that stays in your eye, and you can just periodically fill it from the outside, and it will slowly diffuse. So there's a lot of really interesting technologies out there, and I think a lot of this robotic, high-precision stuff it might make some of these procedures easier to do. I mean, I'm always, whenever I've worked with ophthalmic surgeons, I'm amazed at how steady their hands are. They are so, because they need micron precision, some of these surgeries. And we can make robots that do that, right?
BM: Yes. It's the precision aspect, isn't it? You can deliver ultra-precisely. I love ophthalmology generally, because they're the happiest specialists I ever worked with. They usually have great outcomes. I mean, most of them do cataract surgery and lens replacement, and most of their patients are ecstatic with the results. Great field to work in. But okay, so just getting back, we mentioned some of these procedures. Delivery of drugs, cutting, stitching, cauterization, these are all possibilities at a very small scale, or not really. What are the limits here? What tools we can equip?
BN: Yeah. I mean, I think one of the challenges is anything that requires a lot of force. So stitching is hard. Stitching would be hard for a robot, but maybe you could imagine something that would get there. One of the things we're interested in is occlusions, and that is delivering an embolitic agent. So we talked about trying to remove the blood clot to allow blood to flow. Sometimes you want to stop the flow of blood, particularly deep in some of these structures in the brain, so that it doesn't continue to grow and put pressure on different parts of the brain. And so delivering an agent that can actually, or a device that can stop the flow of blood to particular locations is also interesting. Or filling an aneurysm. If they discover you've got an aneurysm that might burst, we can imagine that we could drive a device into that and somehow fill that up. Right now, if you do that intervastularly, they use a platinum wire that coils, but I think there are things on the horizon where we're going to see polymers. The other way you treat aneurysms, you open up the skull, you go in and you clip it from the outside. Of course, some neurosurgeons are great at doing that kind of thing, but still, if you don't have to get your whole head open, there can be some advantages to going intravascularly and recovering much more quickly then.
BM: Wow. Some of these things are bringing up just the challenges of making these robots. Materials, we started with. I guess you've got people who are physicists and engineers or fluid dynamics people as well for propulsion systems. What's the skill set you're bringing together? How do you make these things? My brain's expanding as we talk.
BN: Yeah. I mean this is one of the great things about being here at ETH. I've run a group here now for 23 years. We've had around 40 people in the group. My co-director is a chemist. I'm a mechanical engineer. Chemistry is obviously important to this, all the materials aspects and characterizing those materials and understanding them. That's a huge part of what we do. And then the physics side, we go down and we have to understand something about fluid dynamics. We have to understand something about magnetic fields and how to generate those and how to combine all these different fields from different electromagnets to get just the right field and field gradient. We also work with doctors closely and spend a lot of time watching surgeries and understanding that, having people come out, spend some time in our lab. And of course, there's a lot of computer science behind all this. I mean, these are robotic systems. Our systems are all based on the robot operating system called ROS, robot operating system that all robots use. So we use the same thing for our clinical or our research systems. And then we do talk to venture capitalists, investors, trying to understand how do they see the directions in this field going and try to convince them of the kinds of therapies we think we can tackle and is there interest there.
BM: Yeah. Gosh. You must have a lot of postgrads lining up to try and get jobs here, surely.
BN: Yeah. I mean, we get a lot of applicants. We get every day, there's several people applying. And I mean, we're in Zurich. I mean, it's a beautiful sunny day here. The mountains are out. You can see the lake here. ETH is a very international place. It gives you a lot of... It's got great resources and it gives you a lot of freedom to tackle big problems.
BM: Nice place to be, I think. And the problems are interesting and they're positive. I mean, they're all about making positive change to people's lives ultimately, when they translate.
Is biocompatibility an issue? I'm just trying to think of... But I guess that gets back to dissolving and metabolizing.
BN: Yeah, biocompatibility is big. And that, over the years, when we were first in this, 20 years ago, we didn't think so much about that aspect of it. We were just trying to figure out how to make these things move and whatever technologies we have, we would use. And we would use nickel for magnetic materials because it was easy to plate or we'd use indium gallium arsenide, nanoribbons and things like that. But then over the years, we started realizing, look, we've got to think about this biocompatibility issue. And that dramatically reduces the materials you can use. But you've got to do it. Although you might be able to show a really cool demo and get people excited, but you're like, wait a minute, that's never going to go anywhere because you're using neodymium iron boron. Well, neodymium iron boron is a toxic material, you can't leave that in the body. And so these things are, they make it a challenge, but like I said, it's...
BM: How do you do the fabrication? It must be almost one atom at a time, the way you build these...
BN: So it depends on what you're doing. A lot of it's nanoparticles. So a lot of our aspect, we got a whole group that's just making nanoparticles. And so there's different techniques there to get those. And we've got our polymer people that know how to, different ways of depositing polymers. About, I don't know, 15, 20 years ago, 3D nanoprinting came about. Nanoscribe hit the market and we were lucky to get one of the first systems. And all of a sudden we could create shapes at the micron scale that we could never have created before.
BM: With multiple materials? Multiple compounds?
BN: With different materials, yeah. And that opened up a whole new possibility for us and looked at all that. But again, as you go down the research path, but then you think, okay, now what do I need to do to translate that? And then one of the things you always have to look at in fabrication is how is this going to scale? I might be able to make one or two devices or maybe a few grams of material, but if I'm really going to scale this, I need to look at much bigger quantities. And so then you also start thinking about the manufacturing in the long term and is it scalable from that sense.
BM: And are they? The ones we're...
BN: Some of them are and some of them aren't. So you get something to work, you realize, okay, that's not scalable. Now what else can we bring in? What other manufacturing technologies might we be able to leverage here to bring it out?
BM: Can I ask, what does a 3D nanoprinter cost? What's it worth?
BN: Around a half a million bucks or so. It depends on how many bells and whistles you got on it.
BM: Not completely off the chart.
BN: No, no. And we get together a bunch of professors. We'll try to pool funds and then we'll go to a funding agency and say, oh, we got this great idea, and we're going to kick in this and can you kick in some money? And so that's one of the challenges.
BM: I desperately want to play with one. I visited a lab in IBM many years ago and they did a sort of a party trick for visitors, but they had a scanning tunneling microscope and they allowed me to reach down and pluck an individual atom off a surface and move it. And there's all this machinery in one room and it allowed me to... And I’ve got to say, it changed my life.
BN: Was it Yorktown Heights?
BM: It was at Almaden in California. And I wrote about it. It changed my life because there's a few things that happened in that lab, but one of the things, they were trying to really impress upon me that I wasn't thinking far enough ahead. Their research was down to that atomic scale when we talk about circuitry, many generations ahead. And how do we build wires that are a few atoms wide and this sort of thing. But that experience of moving and seeing the movement of one atom was just this omniscient sort of feeling. And it changed my perspective on what was possible.
BN: I think Don Eigler is behind a lot of that. So, the Nobel Prize for the scanning tunneling microscope was just down the lake here. IBM Ruschlikon. IBM has a research branch here in just, I don't know, 10 kilometers from us or so.
BM: If I had known, I would have been hammering them with emails trying to get in ...
BN: Yeah. And so they, I don't know, they won it either '86 or '87. They won two back to back, one for superconductors and one for the scanning tunneling microscope. And it was just right up the lake here. You can almost see them from my office.
BM: Brilliant. I love that stuff. Yeah. That it's so inspiring. So, two other technical questions and they relate. So one is … How are we doing? Are we good for time or a little bit more?
BN: Good. Good.
BM: One is just the level of autonomy. These things are robotic in the sense that they do a lot themselves, but in general, the systems we're talking about are monitored very closely external to the body, aren't they? Or throughout the procedure. Would that be a fair description? They're not really truly autonomous. Is that a thought process or is that something we have to go to, true autonomy, to do some of the procedures that you're thinking or?
BN: Well, I think that's the holy grail of micro-robots would be to make them smart enough to figure out on their own where do they need to go and how to get there. We've kicked around some ideas and published some papers and stuff, but I think it's still a long way away.
But what you will see right now in the US, there's a program called ARPA-H for Health. It's like DARPA, the defense group, but this is ARPA-H. And that's one of the things they're pushing is autonomy in surgery. And I think that's an interesting thing to think about because it'll make us rethink some of these surgical procedures for one thing, and maybe we'll come up with better ideas to do them. But also some of these stitching and things like that, they're kind of boring. They're kind of dull. You do them repetitively. And if you can train a system by watching humans and learn how to do it, you can imagine some benefits to that. So, certainly autonomy is on the horizon for surgical procedures and how we can go there. We're always going to want, obviously, a human in the loop.
BM: Sure, in the loop. Exactly.
BN: And the variation in human anatomy and the variation in conditions of the patient, you're always going to need somebody who's really got the judgment, the surgeon. And if the machine can take parts of it over, great. But it's the same problem. I think airline pilots, we've had the same issue. As automatic pilots have gotten better and better, people are wondering how, oh, pilots don't know how to fly anymore. Well, of course they do. But it's just change. But right now, we've got planes that actually take off and land on their own if you wanted them to. But we never want the pilot out of the cockpit, that's for sure.
BM: For sure. But the thing is, the more autonomy, I just imagine the more autonomy we can give, also the bigger the footprint for that type of surgical procedure in lower-skilled areas. So surely that's -- you can take it to smaller developing countries and say, well, there's more autonomy, therefore this is something that can be run by someone without the finer skills or the same level of experience.
BN: No, that's true. We call it democratizing surgery is one of the terms they use for that.
BM: There you go.
BN: But if you have a blood clot and you go to meet a surgeon who's going to remove that, here in Switzerland, you train as a doctor for six years. You go straight into your bachelor's and your master's, you got that. Now, you want to become an interventional neuroradiologist, you have another typically on the order of six, seven years training beyond that. So there's not enough people doing this. And so if you can somehow allow qualified people to do more complicated procedures with less training, you've expanded the number of patients that get treated. And so it's not that we have more doctors than we need, it's we don't have enough doctors with these skills. So if you go into the global South somewhere and we've got maybe somebody that can do a catheterization in the femoral artery or something, now all of a sudden they can maybe connect through Starlink to a surgeon here in Zurich and help guide them in the procedure. And so I think the possibilities are fantastic and I think there's a real need. And these technologies are coming together. When you look at 5G and the communication possibilities for that, you look at Starlink and all these low Earth orbit satellites that are connecting us, all the stuff comes together in interesting ways.
BM: Definitely. I guess related to autonomy is sensory capabilities. That was the other question I've been puzzling over as I look at these things. How much can we equip the actual device with sensing? We can sense where it is externally, as you said, we can follow it, but do they have vision? Are they carrying cameras? And if it has to go beyond cameras, what else can we equip such a small device with? And it was just a pure big question mark for me coming here. What can we or should we … where are we at with that?
BN: Well, we've had over 20 years, we've had capsule endoscopes, these little pills that are given... The imaging one, are what? 11 millimeters in diameter, 29 millimeters long, that have cameras and communication on them. So you can do that. And people are looking at this, people like Gio Traverso at MIT is looking at trying to make more and more complicated devices that can go through a GI tract and do that. So there are sensors being put on the bigger devices. The smaller you go, the harder it is to do these things.
BM: Yeah. Because they're pill-sized.
BN: Yeah. Yeah. So these are actually pretty big. I've got one over here on my desk.
BM: A big glass of water is required.
BN: Yeah. Then you've got folks that have for years have been trying to make them mobile and put motors on them or push them around with magnetic fields. So people are going that direction. I think that'll be interesting. But as you get smaller, then it gets more of a challenge and you have to rethink how we're approaching the problems. We use the word intelligence. We kind of throw intelligence around. I don't think anybody really knows what that means, right?
BM: Yeah, of course.
BN: But we just try to make it behave in interesting ways that help it achieve the given task.
BM: I mean, these things, if they're going to navigate themselves around ... What will be their points of reference? Visual, magnetic. Chemical is interesting. If they've got their own chemical detection, they can go zooming in looking for a source of something.
BN: A lot of times, like around a tumor, there might be a different pH level or a different temperature too in some of these locations. And so now you can start thinking how this device might control itself autonomously to move to a higher pH or something.
BM: Sounds, going into the heart.
BN: Right. Right. Yeah.
And that's the other thing, you go back to nature and you're like, how does a bacteria... Why does a bacteria... First of all, why is it moving? Why has a flagellated bacteria developed this locomotion strategy? How does it sense an environment and what control strategy it does? It's absolutely fascinating. And as an engineer who's been working in the field of controls for well over 40 years, I would never invent a control strategy the way they use this biased random walk to move in directions where life's getting better for them.
BM: But listening to you say that, the answers have to lie there, don't they? It's nature. Nature has to be the inspiration for all of the answers to these questions.
BN: Well, they've had some billions of years to evolve solutions that are pretty interesting. And yeah, it's really fascinating to understand first of all how nature solved the problem and then you look at how it progressed. Now, the problem with nature is it's always got to build on something that already exists. Now, that's our advantage as engineers is we're not as constrained as nature in our solutions. That's it.
BM: So just to finish off, questions I ask everyone really, but is there anything in particular you wish health leaders knew that they don't know about your work? And also, I guess, is there one thing in particular health leaders, policy leaders, regulators, is there one thing they could do that would make your life a lot better, accelerate this process?
BN: Yeah. Well, yeah, there's several things that come to mind. I think one thing with microrobots is, it's this fantastic voyage movie from 1966. People think about it, they think it's far out, but we're really getting to the point where we can do this at human scales, at clinical scales. It's not just stuff under microscopes, now we're able to guide these things within the human body in interesting ways. And so now that's going to allow us to rethink that.
The other thing that I think is extremely exciting is telesurgery and how now we're, with all the communications around the world, we're going to be able to deliver complicated healthcare solutions, complex healthcare solutions to places that just didn't have the capability before. And I think how that gets regulated, how reimbursements are being done, how responsibilities, those are issues that need to be worked out, but they can be worked out.
But I think we're going to see microrobots in humans soon, and we are going to see complex procedures being done by highly trained surgeons from thousands of kilometers away on the patients. And I think that's on the horizon, it's going to come, and if people are aware of it, people in the right positions, they can help kind of grease the skids and help us get there quicker.
BM: And as you were saying earlier, it's all of these systems developing together that are opening up the possibilities. The telehealth, the satellites, all of that.
BN: Exactly. It's a system-level problem. A lot of things have to come together, but we're getting there, and a lot of things are coming together technologically right now that make it look real, look and feel real.
BM: Amazing. Professor Bradley Nelson, thank you so much for having us at the lab, and thank you for those amazing insights.
BN: Thanks, Bruce. It was a pleasure talking to you. Thank you.